Co-production in social care involves care recipients and providers coming together to jointly make decisions and shape how care is delivered. It’s like being part of a collaborative team where every member is essential.
By pooling everyone’s unique experiences and insights, care becomes more personalised and effective.
Dive into this article to explore what co-production really means, its impact on social care, and practical ways to integrate it into your organisation’s approach.

Table of Contents
What is co-production?
Co-production is when people who receive care and the people who provide care work together as a team. They plan, make decisions, and give care together. This way, people who receive care and those not directly involved in day-to-day care are also able to share their own ideas and experiences.
The Social Care Institute for Excellence (SCIE) says this is about changing how care professionals and those who receive care see each other. They treat each other as experts and are guided by each other’s experiences.
The principles of co-production
Co-production in social care is founded on essential principles like equality, diversity, accessibility, and reciprocity, each playing a vital role in making it a truly inclusive and effective practice.
Equality - recognising everyone's opinions:
Equality in co-production starts from the belief that no one is more important than anyone else. Everyone, whether they are receiving care or providing it, brings valuable assets to the table.
These assets aren’t just skills and abilities; they include time, experiences, and perspectives. Achieving equality requires a power shift towards those receiving care, ensuring they have an equal voice in the co-production process.
Diversity - embracing inclusivity:
Diversity in co-production means ensuring that the process is as inclusive as possible. It involves proactive steps to include under-represented groups, such as people from minority ethnic backgrounds, LGBTQ + communities, individuals with communication differences, people with dementia, and those needing substantial support.
Recognising that everyone has multiple facets to their identity is crucial in making co-production truly diverse.
Accessibility - ensuring equal participation:
Accessibility is fundamental in co-production. It’s about making sure that everyone can participate fully and in ways that suit them best.
This includes physical access to meetings or events, as well as making information and language used in co-production accessible to all. Ensuring that everyone has the information they need to participate in decision-making is a key aspect of this principle.
Recognising that everyone has multiple facets to their identity is crucial in making co-production truly diverse.
Reciprocity - mutual benefits and responsibilities:
According to SCIE, reciprocity in co-production is about ensuring that everyone involved gets something back for their input.
This concept is linked to the idea of mutuality, where all parties have responsibilities and expectations. Reciprocity helps build a sense of community and togetherness, making co-production a mutually beneficial process.

The benefits of co-production
Co-production in social care brings a host of benefits, enhancing how care is delivered and received. From improving the quality of care to ensuring it’s efficient and inclusive, co-production addresses various aspects of care.
Let’s explore how this collaborative approach makes a significant difference in social care.
Enhanced quality of care
When people who get care help shape their care, the quality gets better. Co-production makes sure care meets the real needs and wants of the people using it.
Let’s explore how this collaborative approach makes a significant difference in social care.
Improved outcomes
When care users share their own experiences, care gets better. This is because services become more suited to what people really need and want. It’s like when someone really understands you and knows exactly what you need – that’s the kind of service co-production aims for.
Increased efficiency
Co-production makes care more efficient. This isn’t just about saving time and money. It’s about making sure the care really helps in the best way possible. It’s about delivering the right kind of care, at the right time, in the right place, by the right people.
Promoting social inclusion
Co-production is also about bringing people together. It helps break down walls between those who give care and those who receive it. This means everyone understands each other better and feels more connected.
Co-production in practice: Real-world examples
Co-production isn’t just a set of principles; it’s a practice that’s making real changes in social care. Let’s explore these cases to understand the tangible impact of co-production on care delivery.
Example A: Co-production in domiciliary care
In this example, the focus is on creating a care plan that is truly representative of the individual’s entire spectrum of needs and preferences.
It’s a collaborative effort that brings together healthcare professionals, social care providers, family members, and local authorities to deliver care that is not only personalised but also holistic and integrative.
1) Initial assessment and plan creation:
- The individual receiving care works closely with a care planner, usually a professional from a social care provider, to develop a personalised care plan. This is facilitated using specialised care planning software, allowing for a detailed and adaptable plan.
- The person’s daily preferences, routines, and specific assistance needs are discussed. This can include anything from medication schedules to physical therapy requirements and recreational activities.

2) Involvement of healthcare professionals:
- The individual’s General Practitioner (GP) and any other healthcare professionals (like nurses or therapists) are also involved in the planning process. They provide medical insights and recommendations that are crucial to creating a comprehensive care plan. This ensures that the medical and health needs of the individual are seamlessly integrated into the domiciliary care plan.
3) Family and community involvement:
- Family members and close community connections are also included in the co-production process. Their insights into the individual’s preferences, history, and personality can greatly enhance the personalisation of the care plan.
- This involvement also helps in creating a support network for the individual, fostering a sense of community and belonging, which is vital for their emotional and mental wellbeing.
4) Coordination with local authorities:
- Local authorities or council services might be engaged, especially if there are aspects of care that involve community resources, financial support, or legal considerations.
- They ensure that the care plan adheres to any necessary regulations and that the individual can access all the community support and resources available to them.
5) Ongoing review and adaptation:
- The care plan is not static; it’s reviewed and adapted regularly. This might involve scheduled meetings with the care team, including the social care provider, GP, family members, and any other involved parties.
- Regular feedback from the individual receiving care is crucial in this process. Their experience with the care provided guides further adaptations and changes to the care plan.
Example B: Co-production in residential care
In a residential care setting, co-production involves multiple stakeholders working collaboratively to ensure that the living environment and services are tailored to the residents’ needs and preferences.
Here’s how this collaborative process might unfold:
1) Participatory decision-making:
- Residents form a committee or group that actively participates in making decisions about the day-to-day operations of the care home. This could involve choices about meal menus, activity schedules, and communal space usage.
- Regular meetings are held where residents can voice their opinions, suggestions, and concerns. This ensures that their preferences directly influence the living environment and activities.
2) Collaboration with care staff:
- Caregivers and residential care staff work closely with the resident committee to understand their needs and implement their suggestions. This includes adapting care routines, organising preferred activities, and even adjusting meal plans.
- Staff training may include modules on effective communication and engagement strategies to facilitate this collaborative approach.
3) Involvement of family and external health professionals:
- Families of the residents are encouraged to provide input, especially in areas related to personal preferences and history of the residents which the care staff might not be aware of.
- External health professionals, like GPs or specialists who attend to the residents, are also consulted. They provide valuable medical insights to ensure that the care plan is aligned with each resident’s health requirements.
4) Integration with local community resources:
- The care home might collaborate with local community groups, services, or resources to enrich the lives of the residents. This could include organising community events, local outings, or bringing community services into the care home.
- Engaging with local community resources helps bridge the gap between the care home and the wider community, promoting social inclusion and a sense of belonging.
5) Ongoing evaluation and adaptation:
- A care plan in a residential setting is dynamic and is regularly evaluated and adapted based on residents’ feedback and changing needs.
- This might involve periodic surveys, feedback sessions, and review meetings with all stakeholders, ensuring that the care home continues to evolve in line with the residents’ preferences.
Challenges and considerations in implementing co-production
Adopting co-production in social care, while beneficial, presents several challenges and considerations that need careful navigation.
Here’s an expanded look at these hurdles:
Changing how we think:
Care professionals: They often need to shift from a traditional, top-down approach to a more collaborative, client-centred approach. This requires openness to new ideas and willingness to share decision-making power with service users.
Care receivers: Similarly, those receiving care need to embrace a more active role. They’re not just passive recipients of care but key contributors to the planning and execution of their own care services. This shift can empower them but also requires adapting to a new role in their care.
Training and support:
Comprehensive training: Effective co-production requires thorough training for care professionals. This includes understanding the principles of co-production, communication skills, and the technical know-how to use relevant tools and software.
Ongoing support: Beyond initial training, ongoing support is crucial. This could be in the form of regular workshops, refresher courses, or access to resources that help all parties stay engaged and informed in the co-production process.
Power dynamics:
Sharing responsibility: Traditionally, care providers hold more decision-making power compared to those receiving care. Co-production aims to level this playing field, ensuring that care recipients have an equal say in their care.
Negotiating roles: It involves redefining roles where caregivers are as much facilitators as they are providers, and care receivers are active agents rather than passive participants. This requires a careful balance and often a cultural shift within the organisation.
CO-PRODUCTION TIP!
Addressing these challenges is essential for the successful integration of co-production in social care. While it may require additional training to overcome these obstacles, the outcome is a more democratic, efficient, and personalised care system that benefits all involved.
The future of co-production in social care
As we look to the future, co-production is increasingly becoming a cornerstone in the evolution of social care. It aligns perfectly with current priorities like personalising care and leveraging technology, and is gaining support through evolving laws and policies.
Here’s why co-production is key to the future of social care and how it’s set to transform the sector.
- Matching today’s priorities: Things like making care personal and empowering those who receive care fit perfectly with co-production.
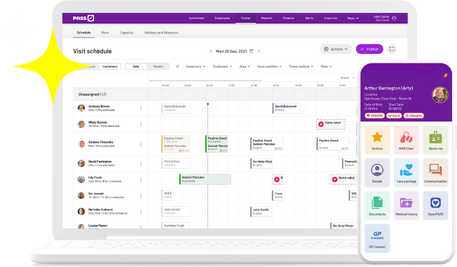
- Technology: As tech gets even better, it’ll help make co-production even more effective. It makes planning care and getting everyone involved easier, especially with tools like care management software.
- Laws and policies: Laws like the Care Act 2014 are starting to support co-production. This kind of backing is really important for making co-production a regular part of social care.
How technology enhances co-production
Technology is playing an increasingly important role in co-production in social care. Here’s how:
- Care management software: This software makes communication between care users and providers easier. It helps make sure that what people needing care say gets heard and used in planning their care.
- Care planning software: This tool is all about creating care plans that are just right for each person. It can change and update plans easily, making sure care stays responsive for the person’s needs.
- Roster software: This kind of software is great for organising who does what in care settings. It helps make sure that the right people are giving care at the right time.
READ MORE
For more detailed information on these topics, the Social Care Institute for Excellence (SCIE) and the NIHR School for Social Care Research provide extensive resources and insights.
Final thoughts on co-production
Co-production in social care is important. It’s not just a set of principles; it’s changing how care is done. It’s all about working together – people who get care and those who provide it. Everyone’s experience and ideas matter.
This way of doing things makes care more about everyone, works better, and is more effective. As we go forward, using co-production is going to be important for tackling the challenges in social care and making sure care is what people really need and want.
Co-production FAQs
How does co-production impact the efficiency of social care services?
Co-production makes care more efficient. It helps match care with what people really need. This can mean less spending on things that aren’t needed and better care from the start.
Can co-production be applied in all care settings?
Yes, co-production can work in lots of different places like at home (domiciliary care), in care homes, and in community services. It’s flexible and can be used in many types of care.
What role does technology play in co-production?
Technology is important in co-production. Care management software helps everyone communicate, make care plans that fit just right, and manage everything efficiently.
How does co-production enhance the quality of care?
Co-production makes care better because it uses what people getting care know and want. This means care services really meet the needs of people using them, which makes the care much better.