As social care professionals, we know the importance of communication in health and social care. Whether we’re communicating with service users, colleagues, family members, or other professionals, we need to provide accurate, reassuring, and timely information.
Depending on our audience, we may need to communicate in different ways. For example, some of our clients may not be able to understand written messages, or may struggle to communicate verbally with us.
However, written communication is crucial for incident reporting, and electronic communication such as care planning software means that colleagues can communicate clearly with each other.
In this article, we’ll explain why communication is important, different methods of communication in health and social care, barriers to effective communication, and finally, how we can achieve good communication.

Table of Contents
Why is communication in health and social care important?
Communication is important in any sector. Everyone needs to ensure that their colleagues, clients, and other stakeholders hear and understand them.
But communication in health and social care is especially crucial. Our clients trust us with their health, their independence, and, in many cases, their lives.
We have a responsibility to provide them with the best service possible. If we make mistakes, they can have disastrous effects for our service users.
We can provide a safe service by communicating well with our clients, their families, our colleagues, and other professionals.
Communicating with service users
Service users are the heart of every care service. Whether our service users are older people, children, or adults with disabilities, we need to communicate with them in a person-centred way.
Every day, we talk to service users about a variety of topics – everything from personal care and consent to food preferences and the weather. At times, we may need to communicate information about legal matters, care finances, and other sensitive topics such as end-of-life care.
The people we support may experience a wide range of emotions, or exhibit challenging behaviour. Some of our clients may not be able to communicate verbally – for example, they may have physical or mental health conditions that make speaking, hearing, or processing difficult.
As care workers, it’s our responsibility to ensure we still communicate effectively with them.
Communicating with families
In some cases, we also need to communicate with service users’ families. We may do this in a variety of situations, including:
- If the person we support is a child, and we need to speak with their parents or guardians.
- If the service user does not have mental capacity, or a relative has medical power of attorney.
- When we are conducting a care assessment or review.
- If a family member comes to us with concerns or needs emotional support.
- When family members visit their relative and we are present.
- If family members pay for or arrange their relative’s care, and we need to discuss changes to the service or fee structure.
- If we need to relay urgent news about their relative’s health.
Depending on the situation, the communication might be anything from a quick casual chat to a pre-planned meeting or a formal letter.
Like all communication in health and social care, discussion with families may be challenging or emotional. Some of the information they receive and situations they experience may be difficult to process.
But with the support of new technologies, such as openPASS, our friends and family portal, regular and reassuring lines of communication can be opened in real-time.
Communicating with colleagues and other professionals
Whether we work in home care, residential care, or any other health or social care setting, we need to communicate with colleagues.
It might be as simple as exchanging small talk at the start of a shift. Or something more involved, like working together during a care call, conducting a staff member’s performance review, running training sessions, or sending emails or care rotas to colleagues.
Communicating with colleagues is a crucial part of providing good care, being a supportive employer, and maintaining a safe and friendly working environment.
But it’s not just colleagues. Other professionals we communicate with may include:
- Social workers
- Inspectors
- Pharmacists
- Doctors, nurses and paramedics
- Opticians and audiologists
- Physiotherapists
- Occupational therapists
We may need to give them information, or ask for information. As we know, many of these professionals are also busy, so it’s helpful to have templates or electronic methods for them to provide the data we need.
Methods of communication in health and social care
Depending on your audience and the situation, you may need different methods of communication. Successful care workers, managers and leaders need a variety of different communication skills in health and social care.
Verbal communication in health and social care
For many situations, verbal communication is the easiest and quickest option. Verbal communication involves words – usually spoken, but sometimes signed.
You see verbal communication in health and social care in a variety of scenarios, such as:
- Most care assessments and reviews involve discussion between the client, family members, and care team.
- Care workers providing personal care will usually talk to their clients throughout – both about the activities they’re doing, and also as part of providing companionship.
- Family members may ask about their relative’s condition or behaviour when they see carers.
- Many care teams will have a line-up or handover between shifts, where they raise any issues that occurred in their recent care visits.
- If a GP, district nurse or other healthcare professional visits a service user, a care worker or family member may explain their condition or the situation.
Verbal communication doesn’t have to use English. If a client is more comfortable speaking another language, a care organisation can try to make sure that their carers also speak their preferred language. Alternatively, they may prefer to have an interpreter present where possible.
If a client is unable to communicate with spoken words, they may use a sign language, such as British Sign Language (BSL).
Non-verbal communication in health and social care
Just as important as verbal communication in health and social care, however, is non-verbal communication. Non-verbal communication is a way of communicating without speech or writing.
Some clients may be non-verbal or pre-verbal. But this doesn’t mean that they can’t communicate.
Non-verbal communication in health and social care may include:
- Pointing
- Nodding or shaking the head
- Other gestures, including waving or giving a thumbs up
- Facial expressions, such as smiling or frowning
Anyone might use these forms of communication – they’re a regular part of most spoken or signed conversations. For example, carers working together on care calls may find that they naturally use non-verbal communication when helping clients with tasks such as lifting, dressing, or washing.
However, some clients, especially those with severe or complex learning disabilities, autism or dementia, may not be able to communicate verbally. Working to understand their non-verbal signals is an important part of communication in health and social care.
Written or electronic communication in health and social care
There are many situations where written communication in health and social care is necessary.
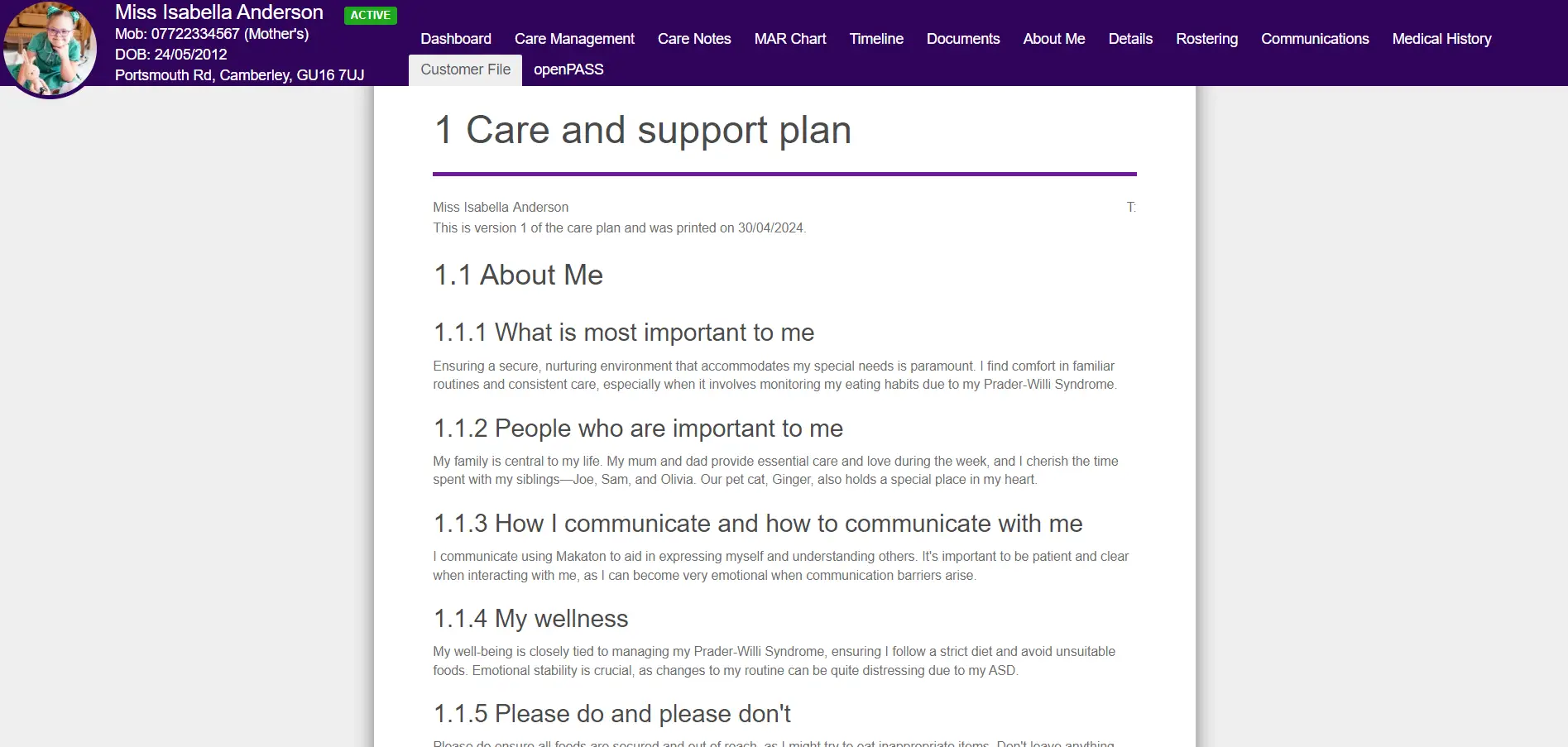
In general, if you or someone else may need to refer back to it later, written or electronic communication is the best choice. This is true whether your audience is clients, families, colleagues, professionals, or even yourself or inspectors at a later date.
You may need to send written communications to clients or their families to advise them of changes to the service, such as fee increases.
Care workers need to ensure that they are accurately reporting with clear digital records. Accurate reporting keeps service users safe, holds staff accountable, and helps organisations provide evidence to CQC and other regulatory bodies when necessary.
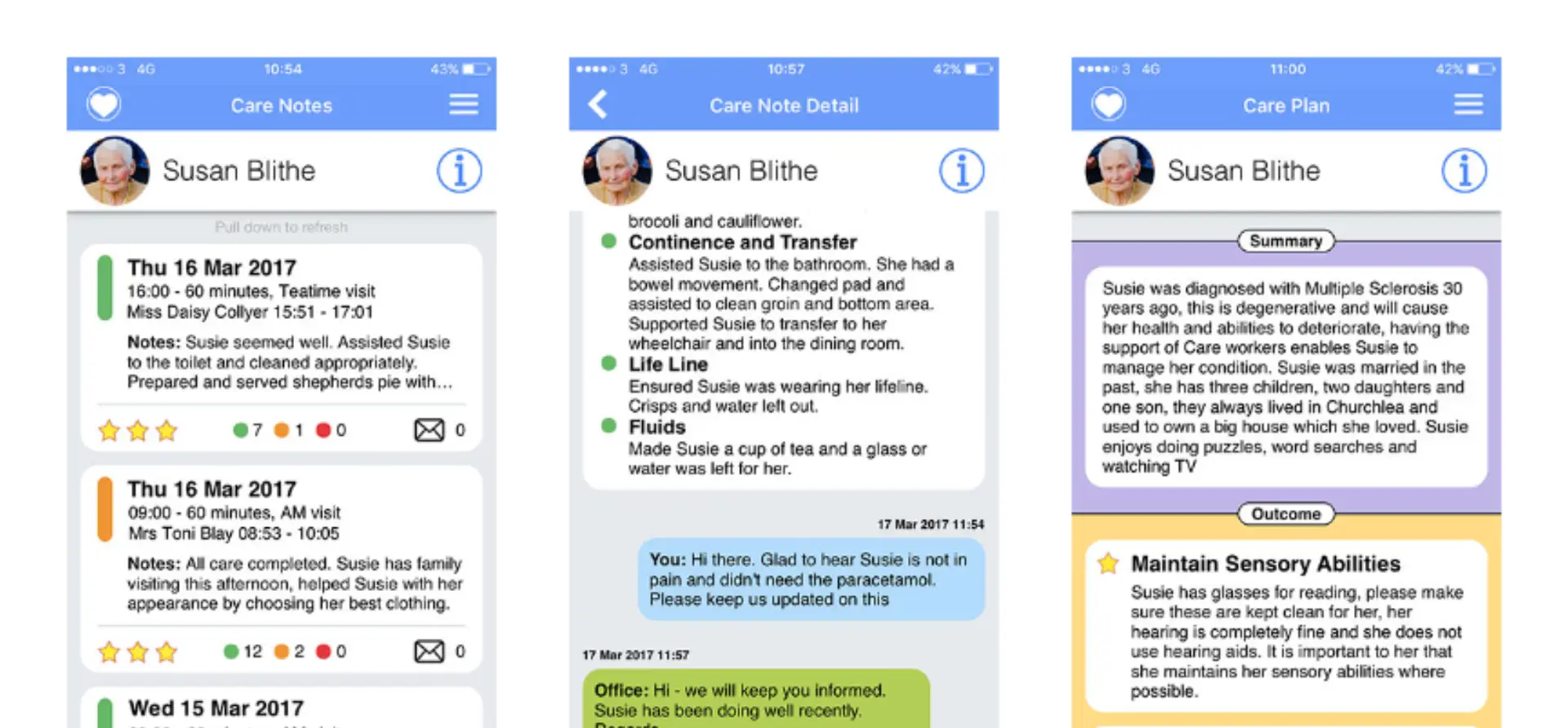
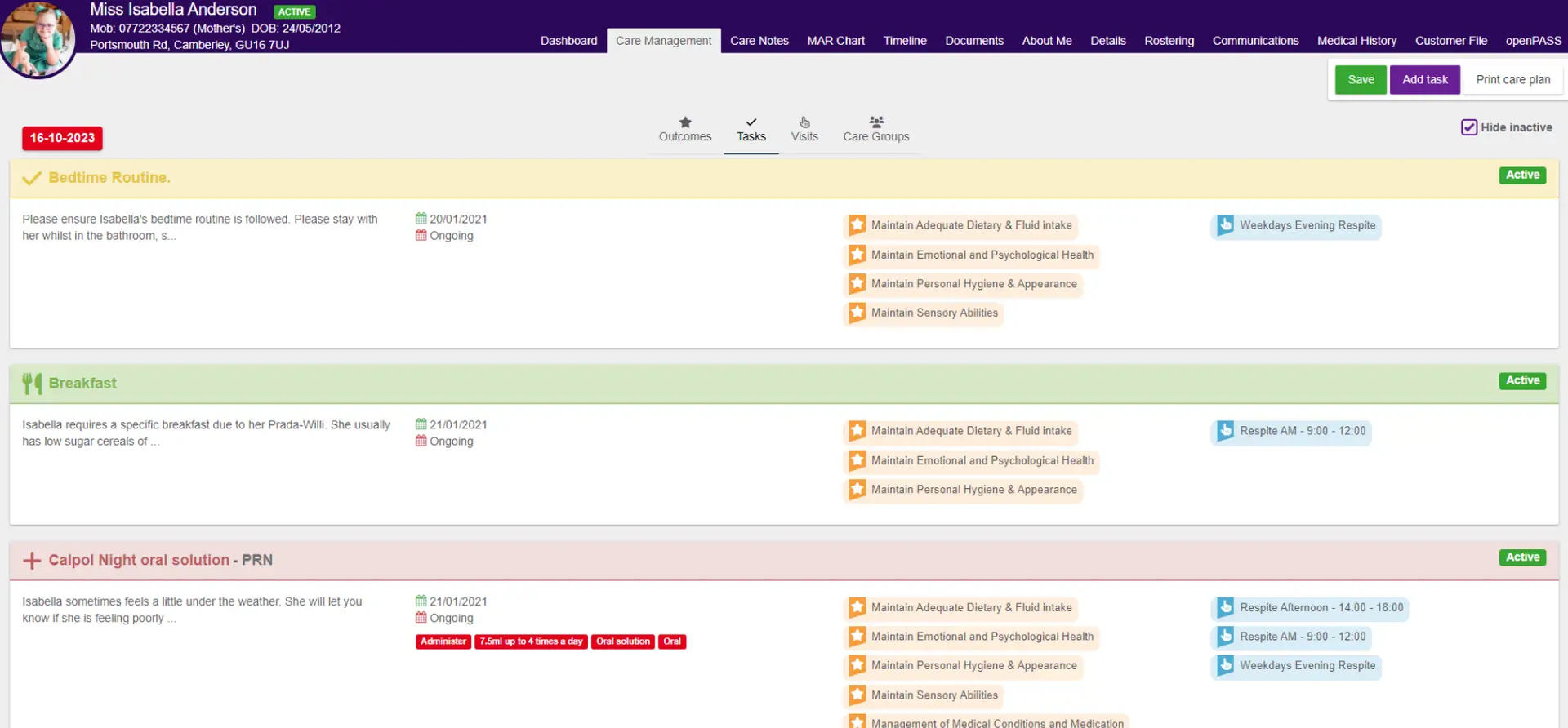
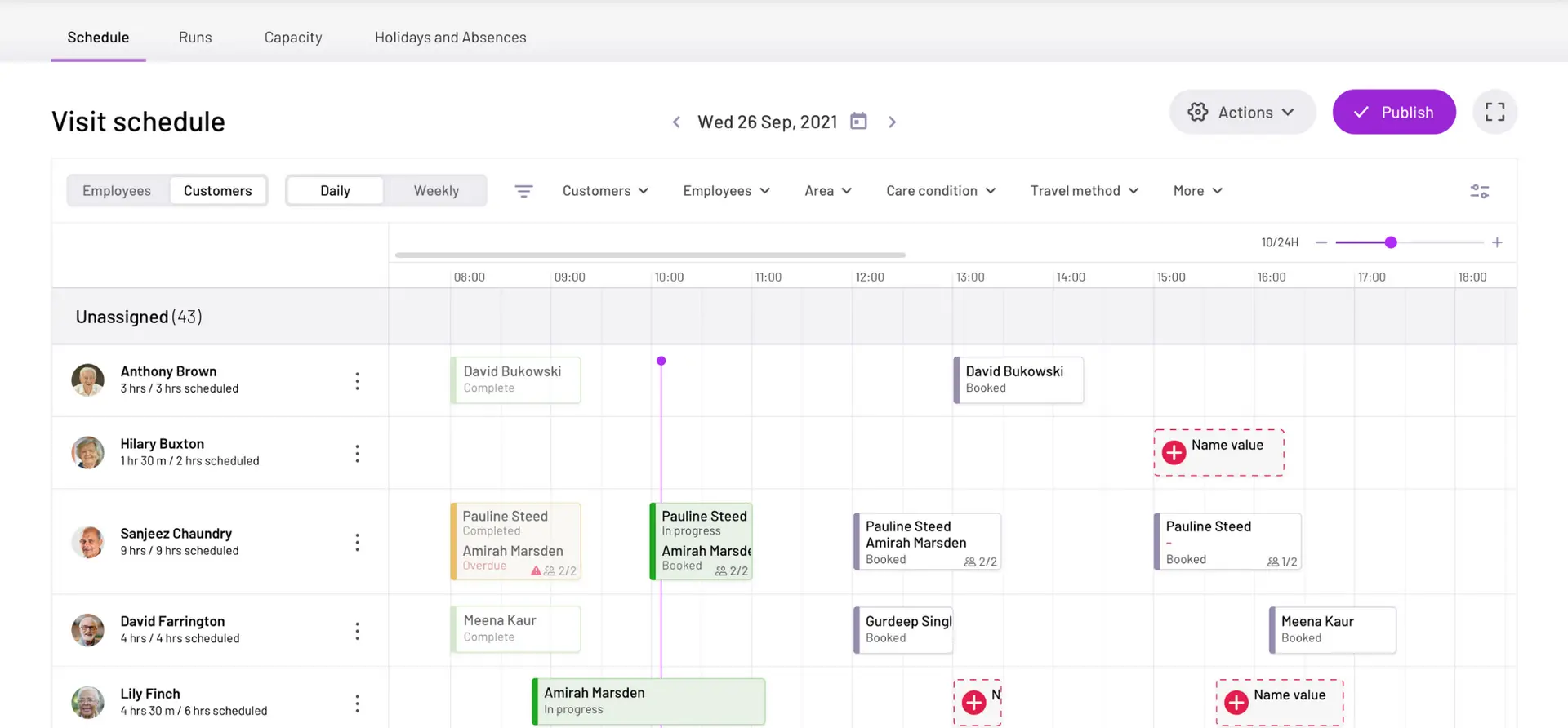
Using Digital Social Care Record systems, such as dedicated home care software or care planning software makes lots of tasks easier for care workers. Instead of relying on paper care plans, records, and rotas, electronic solutions offer many advantages, including:
- Eliminating the risk of losing or damaging paper records.
- Notes and updates sync up on all carers’ devices, meaning that everyone is always using the latest version.
- Voice-to-text options mean that carers can record notes without needing to write or type.
- Colleagues can communicate easily with each other – especially useful for home care workers, who may not regularly meet up.
- Medication databases and Electronic Medication Administration Record Systems (eMAR) can alert care workers to potential issues and give further information when needed.
- Family members can receive instant updates when necessary.
Software such as GP Connect even makes life easier for other professionals, allowing care workers to instantly access GP records, without needing to contact the GP each time.
Barriers to good communication in health and social care
Unfortunately, sometimes it’s hard to communicate easily. Whether it’s with service users, colleagues, or other professionals, we can sometimes struggle to make our message understood – or even find time to communicate.
This might be due to:
- Cultural differences or lack of a shared language
- Communication difficulties as a result of a health condition or learning disability
- Time constraints
- Moods, emotions, and attitudes
- External factors, such as background noise impeding hearing, face masks affecting lip-reading, or similar
However, as professionals, it’s our responsibility to find a way to achieve effective communication in health and social care wherever possible.
How can we achieve effective communication in health and social care?
Effective communication means that the audience understands the message and can respond as necessary. That might be as simple as a carer asking what a client wants to eat and receiving an answer, or as complex as explaining a service user’s symptoms to a medical professional.
Good leadership in social care involves fostering a culture of open and effective communication.
We can do this in a few ways:
- Make sure that scheduled care calls are long enough for care workers to communicate well with clients. You may also need to use translators or schedule care workers who can easily communicate in a client’s preferred language. A smart care rostering system can assist with this.
- Ensure that written communication is accessible, especially for service users and their families. Do they need letters or emails to be translated into another language? Would visually-impaired service users prefer letters in Braille, or do clients with learning disabilities need letters in simplified English?
- Use electronic communication systems for staff and families where possible. They can save time and improve service user safety.
- Try to be accurate and transparent in all your communication. In addition, you should, where possible, give people enough time to process information, especially if it’s something that requires them to take action or may be difficult to hear, such as a new staff rota or a poor performance review.
- Check how people would prefer to receive written or electronic communication. Are clients able to download apps or receive emails, or would they prefer letters? When communicating with busy fellow professionals, what framework allows them to respond quickly?
- Offer training for staff – both in communicating with service users, and in accessing any communication systems used by your organisation.
Like many aspects of health and social care, communication must be driven by the situation.
As this guide is all about communication, we’ll now throw it over to you. How do you think we can achieve good communication in health and social care? Share any tips, thoughts or advice by using the social icons below.