In this article, we’ll look at what empowerment in health and social care is, some of the key issues, the importance of empowerment, and some strategies that can be used to empower individuals.

Table of Contents
A quick note on empowerment in social care
Whether you work in residential or domiciliary care, the importance of empowering individuals in health and social care can’t be overstated. Promoting your clients’ autonomy is a huge part of providing good care.
As care professionals, you know that some of your clients’ lives may have changed a great deal in a very short time.
Many of your service users have had choices taken away from them in the past. They may not have been trusted to make their own decisions, even about small issues, especially if they’ve lived in care homes for a long time.
However, everyone has the right to make decisions about their own lives, and empowerment in health and social care can lead to improved health outcomes and greater satisfaction with the care they receive.
The definition of empowerment in health and social care
At a glance:
Empowerment in health and social care refers to allowing service users to have more control over their lives.
Empowerment is a key part of providing person-centred care. For most people, being at the centre of their own care journey means taking an active role and making their own choices.
Those choices might be about small things, such as what clothes to wear or what to eat, or bigger topics, such as whether to take medication or receive treatment.
Depending on an individual’s circumstances, this may mean making decisions about their care, such as when and how to receive a service, or other decisions, such as being involved in relationships.
Service users should be informed about their options and their rights, so that they can make informed decisions where possible. They should feel valued and listened to when they speak up and self-advocate.
Staff members should respect the autonomy of their service users, and encourage them to be independent when possible.
The importance of empowering individuals in health and social care
There are many benefits of empowerment in health and social care.
Studies have shown that empowered individuals are more likely to experience better health outcomes. As empowerment can also improve self-esteem and confidence, this makes sense – there are well-known links between mental and physical health.
Service users who are empowered to make decisions regularly report greater levels of satisfaction with the care they receive. If an individual has been involved in the production of their care plan, they’re likely to agree with the activities and outcomes included in it.
In addition, service users who are engaged with the decision-making process are likely to provide thoughtful feedback about the care they receive. This feedback can lead to changes and improvements within the organisation, allowing you to provide a better care service.
The benefits of empowerment in health and social care aren’t just for service users, though.
Staff members are more likely to report higher levels of job satisfaction. And that’s understandable – providing care for individuals who are engaged with the process and seeing positive outcomes is rewarding.
All care professionals know that it can be a difficult job at times, and being able to provide a positive work environment will set your care service apart.

Factors affecting empowerment in health and social care
That said, while the importance of empowering individuals in health and social care is clear, there may be factors that make it more difficult at times.
This doesn’t mean that empowerment is impossible, though. As with many aspects of health and social care, every situation is individual.
There’s no one size fits all solution, and care professionals regularly need to think on their feet or adapt situations to suit service users and their individual needs.
Concerns about understanding
Empowerment in health and social care can’t happen in a vacuum. Service users should be informed about their options and choices, so that they can make an informed decision.
However, many individuals that you support will have conditions that make it harder for them to make their own decisions.
Conditions such as dementia or learning difficulties may make it harder for service users to make decisions for themselves.
They may not always be able to understand the impact of some of their decisions, or they may not be able to make informed decisions at all – particularly if they’re not able to meaningfully engage with information about their options and rights.
Where possible, individuals should be encouraged to be part of the decision-making process during their care journey.
The Care Act 2014 says that decision-making should begin with the assumption that service users are able to participate, and are best placed to judge their own well-being.
Concerns about independence
Individuals with mobility difficulties or fragile health conditions may feel that they don’t have the independence or physical ability to make some decisions.
In this situation, it may be important to distinguish between independence and autonomy. Independence refers to being able to do activities alone, whereas autonomy refers to being in control.
While some service users may not be able to do activities independently, their carers can still respect their autonomy, and follow their wishes where possible.
For example, even if an individual can’t dress themselves, they may still be able to choose their own clothing, and their carer can follow their wishes about styling their hair, shaving, or applying makeup.

Concerns about decisions
For some individuals, decision-making may be a cause of stress – particularly if they haven’t had many opportunities to do this in the past. Regular communication and reassurance can help.
Concerns about risk
Some individuals may make decisions that care professionals may consider risky or unwise. However, it’s important to consider that providing the right support and empowerment isn’t about removing risk entirely.
Instead, it’s about ensuring that your service users are supported to make informed decisions about their own lives.
You may be able to mitigate concerns with risk assessments, discussions with the service user and their family, if appropriate, and risk management strategies.
For example, if an individual would like to continue smoking, the care team could plan care visits to coincide with their smoking times, to ensure that they aren’t at risk of falling asleep alone while smoking.
Organisational constraints
As all care professionals know, there are never enough resources.
For example, you might have multiple service users who would like a care visit at 7am, but not have the staff to accommodate them all at the same time. Your care team may be able to handle some visits at 6.30am, some at 7am, and some at 7.30am instead.
There may also be times when you want to provide additional services but lack the staff or budget to do so.
Involving service users in the care planning process and being honest with them about any limitations can help.
Location
Empowerment may look different for all service users, but especially for care home residents compared to home care clients.
Many people receiving home care choose this option because they want greater independence.
However, some people may not have a choice about moving to residential care – for example, their previous home may be unsuitable for someone with mobility issues, or they may need round-the-clock nursing care.
Wherever a service user receives care, they may still benefit from making decisions about their own care journey.
In the past, many residents of care and nursing homes followed similar schedules, ate similar meals, and had little control over their own lives.
However, now that we know the benefits of empowerment in health and social care, it’s important to try to support all service users to make their own decisions and have autonomy.

Strategies used to empower individuals in health and social care
Now you’ve heard about the benefits of empowerment, how can you help to ensure that it’s part of your organisation’s culture?
It should come from the top down, and your organisation’s processes and policies should encourage empowerment and the promotion of independence.
Your staff team should receive regular training that promotes the idea of empowerment. They should be encouraged to listen to clients, and respect their choices. Some training sessions that help may include:
- Equality and diversity training
- Person-centred care training
- Communication training
- Mental capacity training
In addition to training your current staff team, you may want to involve service users in your recruitment processes.
This may include helping to produce job descriptions, as well as being involved in the interview process and giving feedback.
It’s important to encourage communication between the staff team and service users. This gives care workers the chance to check in with clients, and clients the chance to speak up and self-advocate when necessary.
Depending on your service users and their preferences, you may wish to provide several different methods of communication. Some individuals may be more comfortable speaking to a care worker, whereas others may prefer to communicate in writing.
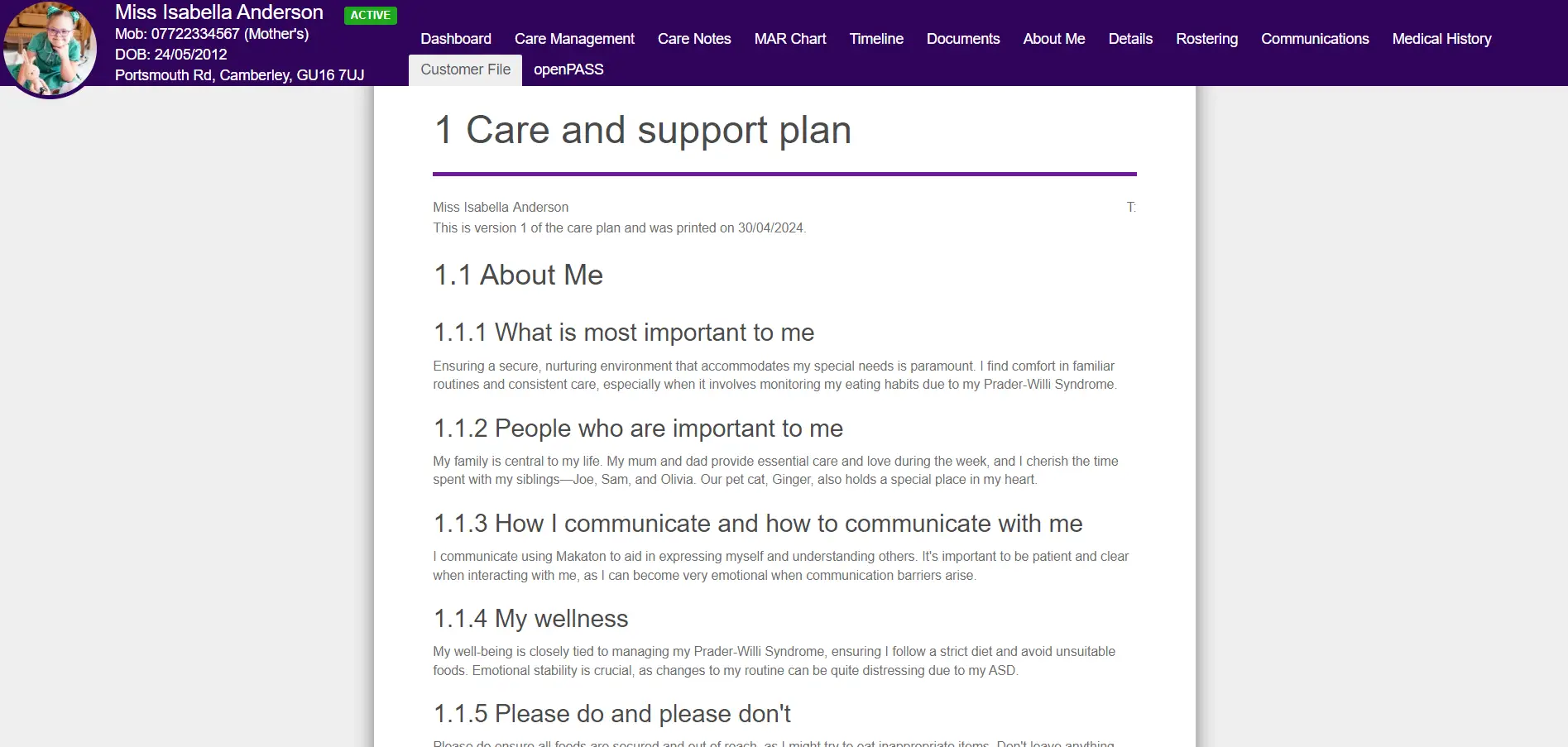
Empowerment in health and social care should start from the very beginning. An individual should be involved in the production of their care plan, or in the planning of services that could affect them – a process called co-production.
Service users may have strong preferences about the gender of their care worker, for example, or the timing of their care visits.
Empowering and promoting independence in health and social care
As a care professional, you’re probably already empowering your service users every day with small choices. In your organisation, there are probably already many examples of empowerment in health and social care.
Technology, such as care management software, may be able to help you empower your service users even further. Digital Social Care Records can help you create truly personalised care plans, working with your clients to give them autonomy and independence where possible.
Article by:

Jessica Slattery, Digital Social Care Expert @ PASS
Jess and her team have worked with more than 1,200 social care businesses, providing expert advice on Digital Social Care Record (DSCR) systems, resulting in thousands of hours saved, improved CQC ratings, and better quality of care for the people they care about.