Medication errors are a critical concern in health and social care, impacting service quality. In this guide, we’ll cover strategies for managing errors like incorrect dosages, missed medications, or service user refusals, helping professionals minimise risks and improve care outcomes.
Table of Contents
A quick note on medication errors
What would you do if you gave the wrong dosage of medication to a service user? Do you know what to do if a service user spits out medication?
As a care worker, you’ll probably need to administer medication at some point in your career. When you do this, you should be aware of medication errors, the possible consequences, and how to avoid them.
Medication errors range from giving the wrong dosage to a service user spitting out medication. Basically, it’s anything that interferes with ensuring that your service user gets the medication they need.
In this article, we’ll talk about the most common medication errors, what to do if they happen, and how to reduce the risk of medication errors in future.
⚠️ Call 999 immediately if you’ve made a medication error and the service user is having an obvious reaction.
Signs of an emergency may include:
- seizures
- shortness of breath or being unable to breathe
- sudden confusion, drowsiness or being unable to wake up
- chest pains
- vomiting or diarrhoea
- very fast pulse rate
- sudden rashes, swelling or itching
What are the most common medication errors?
Medication errors can occur at any time when caring for an individual. A doctor may prescribe the wrong medication, a pharmacist may prepare or dispense the wrong medication or dosage, or a care worker may make a medication error while supporting the service user.
Here, we’ve put together some examples of medication errors that might occur while you’re providing care – and how to respond should they happen.
Common scenario 1: the wrong medication is given
When someone talks about medication errors, this is the one you probably think about: giving a client the wrong medication.
This common medication error usually happens when a service user has a lot of different types of medication, or when a carer has many individuals to support.
It’s easy to see how it can happen, especially if the care worker is in a rush. However, this is a particularly dangerous error, especially if the medication was prescribed for a different person.
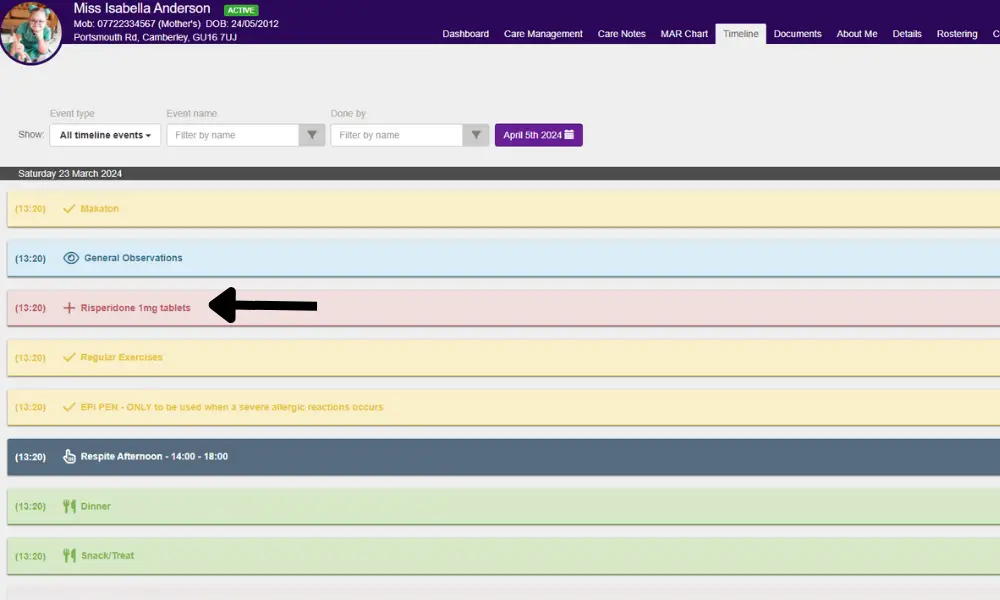
A comprehensive digital care planning system that provides care workers with instant access to up-to-date care records on any device can significantly reduce the risk of common medication errors. By ensuring that the most current care requirements are always at hand, these systems enable care workers to administer medication accurately and confidently, no matter where they are.
Common scenario 2: the wrong dosage of medication is given
As with giving the wrong medication, giving the wrong dosage of medication often happens when service users have lots of different medicines, as well as when carers are rushed and supporting many clients. It may also happen if a client’s care plan isn’t very clear – especially if it’s hand-written and hard to understand.
It’s important to always follow the doctor and pharmacist’s instructions exactly. However, sometimes, a carer gives the client the wrong amount of medication – either too much or not enough.
Both of these can be very dangerous, depending on the medication and the individual’s condition.
With the support of digital social care technology like GP Connect from PASS, care providers can access real-time digital GP health records of service users. This immediate access helps prevent medication errors and ensures that care workers have the most accurate and current information, improving the overall quality of care.

Common scenario 3: the medication is administered at the wrong time
Giving medication at the wrong time often happens when care visits are delayed, or when timings change for other reasons.
Your client’s medication may have instructions such as:
- Take every X hours
- Take before food
- Take after food
- Take at the same time every day
It’s important to follow these instructions exactly. Medication may interact with food, or upset a someone’s stomach if taken at the wrong time. If medication is given too early or late, it could make your client ill.
Investing in a digital care roster system ensures that care visits are perfectly aligned with the service user’s medication schedule. This alignment helps maintain consistency in administering medication at the right times, reducing the risk of missed or delayed doses and ultimately enhancing the quality of care provided.
Common scenario 4: the medication is given via the wrong method
Giving medication in the wrong way may happen if the care plan or medication instructions aren’t very clear. It may not be immediately obvious whether a tablet is to be chewed, swallowed whole, or left to dissolve on the tongue.
As with giving the wrong medication, giving medication via the wrong method can also happen when a care worker is very busy, rushing, or has a lot of clients to support.
Over the course of your care career, you may need to administer a range of medications, including:
- Medication to be chewed and swallowed
- Pills or capsules to be swallowed whole
- Pills to dissolve on or under the tongue or inside the cheek
- Creams or patches applied directly to the skin
- Drops administered in the eyes or ears
- Subcutaneous, intramuscular, or intravenous injections
- Inhalers
This isn’t a comprehensive list, and you should always double-check what the instructions are for your client’s medications.
Common scenario 5: the medication is missed
Medication might be missed for a variety of reasons, including:
- Cancelled or missed care calls
- Rushed care calls
- Poor record-keeping, leading the care worker to believe the medication has already been administered
- The service user is too drowsy or ill to take their medication
- The service user spits out medication, or refuses to take it
Alternatively, the service user may agree to take the medication, but vomits immediately after. If this happens, it can often be assumed that the medication hasn’t taken effect.
An electronic medication administration record system, or eMAR, enables care providers to accurately track what medication is given and when. This system helps ensure that medications are administered correctly, reducing the risk of errors and providing a clear audit trail for every dose given.

Common scenario 6: the medication is repeated
Repeating medication is most likely to happen due to poor record-keeping. If a carer hasn’t recorded administering medication, another carer may give the dose again during a later care visit.
It may also happen if the client is taking their own medication without support.
Care management software improves record keeping and communication, especially for remote care visits. It ensures that all relevant information is accurately documented and easily accessible, facilitating seamless coordination between care professionals.
What should you do if medication errors happen?
If you’re involved in a medication error, it’s crucial to be honest and open about the situation, and seek help as soon as possible.
Depending on your role, you may have different responsibilities after a medication error.
How to manage medication errors as a care giver
If you have made a medication error, don’t panic. The most important thing to do now is to limit the damage and seek help quickly. Panicking will waste time and could make things worse for your client.
Get medical help for your client as soon as possible. Depending on the situation, this may involve:
- Calling 999 if the service user is experiencing a reaction to the medication or you believe that they’ve taken medication that could be harmful to them
- Making an appointment with your client’s GP, practice nurse, or other specialist
- Speaking with a pharmacist
Talk to your supervisor about the error. It’s important to do this as soon as possible, even if it’s at night or a time when they aren’t on shift. Your supervisor will probably need to ask you some questions about what happened and why.
Make sure that you document everything as part of your incident reporting. This could include:
- What happened before you made the medication error – was the shift busy or did the service user have new medication on their care plan?
- What exactly the error was – was the wrong medication given, did you give the wrong dosage of medication, or something else?
- Did the service user have any physical reaction?
- What actions did you take upon realising the error?
- Did you take advice from any healthcare professionals – when did you speak to them, what were their names, and what did they advise?
- Did you call an ambulance or attend A&E with the service user, and what happened there?
Most importantly, learn from this error. You’re not the only person to have made a medication error – studies say that there are more than 200 million medication errors each year within the NHS alone.

How to manage medication errors as a care manager
As a care manager, your work begins before a mistake happens. You need to foster a culture of openness. It’s important that your staff team know what to do if they make a medication error, and that they’re confident to talk to you.
After medication errors happen, there are a few key actions to take.
- Check on the service user. Have they received medical attention? How are they feeling, physically and emotionally?
- Contact the service user’s family or next of kin, if necessary.
- Investigate the incident. Why did it happen, and is there anything you can do to prevent this happening in future?
- Report the incident. Depending on what happened, you may need to report the incident to the CQC, someone higher up in your organisation, or other relevant authorities.
Your organisation may have other processes and policies to follow, and we’d encourage you to read up on these before an incident happens.
How to prevent medication errors
As a carer, every time you administer medication, it’s essential to follow the ‘Six Rights‘ framework to ensure safety and accuracy:
Right person: Always double-check that the medication is being given to the correct service user. Misidentification can lead to serious consequences, so verify their identity using multiple methods, such as their care plan, name, date of birth, or a photo ID.
Right medication: Ensure that the medication you are administering matches the prescription. This involves checking the name of the drug, its strength, and its form (e.g., tablet, liquid, injection). Be particularly vigilant if the medication names look or sound similar to others.
Right route: Confirm the correct method of administering the medication, whether it’s oral, topical, inhaled, injected, or another route. Administering medication through the wrong route can affect its effectiveness or cause harm.
Right dose: Check the prescribed dosage carefully. This includes understanding the exact amount, the measurement units (e.g., mg, ml), and any special instructions for dosing. Administering too much or too little medication can lead to ineffective treatment or adverse effects.
Right time: Timing is crucial in medication administration. Some medications need to be taken at specific times of the day or with certain intervals between doses. Ensure that the medication is given at the correct time as per the care plan to maintain its effectiveness and avoid potential side effects.
Right to decline: Service users have the right to refuse medication. It’s important to respect their autonomy while also understanding the reasons behind their refusal. If a service user declines medication, document the refusal, inform the care team, and seek advice on how to proceed.
If all of these conditions are met, you should avoid most medication errors. As a care supervisor or manager, you should give your staff team the tools to get it right every time.
Dealing with medication errors: key takeaways
- Make sure that care staff are trained on how to administer medications and read care plans. Do they all know what to do if wrong medication is given to a customer, or what to do if a client spits out medication?
- Use an eMAR system, to keep comprehensive medication records and avoid misreading handwriting or losing paper-based medication administration records.
- Ensure that carers have enough time for each care visit.
- Learn from errors. When they do happen, see if there are any common trends, and if there’s anything you can do to prevent future incidents.
Finally, make sure that you foster a culture of openness and honesty, so that your team feel confident reporting any issues.